Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…
CMIO Rant with … Dr. Andy
The Problem List: Foe or Enemy?
By Andy Spooner, MD

I love the problem list. But I hate it, too.
I love that I can take a few seconds in the course of clinical care to deposit a problem into a list that ensures that I will not fail to address the matter as care progresses. A patient’s mother says that her child, who is being admitted for pneumonia, has seen a private allergist for an “immune system problem.” She describes no particular symptoms or treatment for this this problem, but she thought she should mention it to me, the admitting hospital physician.
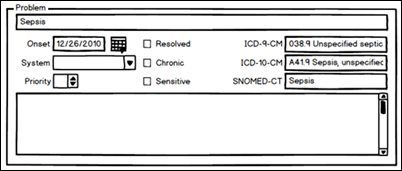
Sounds like something to add to the “do” list. What I need to “do” is to clear up ambiguity and make sure I understand how this issue affects care. So I turn to the computer (yes, right in front of the patient!) and add:
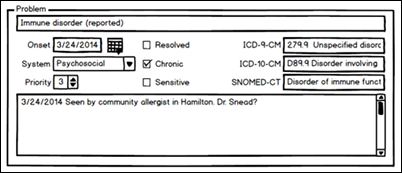
… to the problem list.
(By the way, this is NOT how my EMR records problems. It’s intended to be a vendor-neutral depiction of how one might do it. I used a great program called Balsamiq Mockups—a handy tool when you want to convey a user-interface concept—to make these pictures.)
Later on, after I get a bit more information, I clarify this and add some further detail:
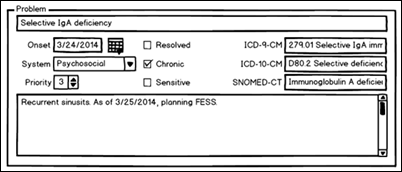
Total time investment: One minute.
Return on investment: This clinical issue is now part of the record and will be part of all future presentations of summary information on the patient. I can pass on this information in handoffs and in record sharing. I can be sure to address it with the patient and family. I can insert it—and all other problems—into my note automatically, if I want, and have instant documentation of the complexity of the patient. I can arrange the order by priority, by organ system, and by whether it is a hospital problem currently.
Larry Weed would be proud.
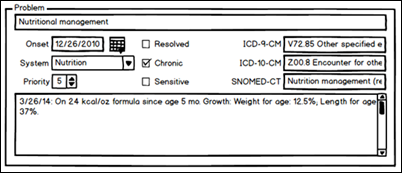
Another patient comes in with a stack of papers from a referring hospital. I paw through this mound and add a couple items to his problem list:
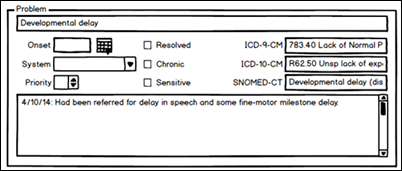
(I am a pediatrician, after all.)
You get the idea: Every time something new hits my radar, I tack it to the problem list.
Why?
- I can, in the start-and-stop world of hospital care, keep up with all of the issues that affect each patient.
- I can insert all of this information, along with necessary comments, into any note that I write. Instant assessment and plan. Instant support for my E & M code. And no necessity to copy my notes forward, in violation of the latest OIG and AHIMA dire warnings.
- I can go over each issue with the parents, and they can be fully informed of the things I am worried about. By looking at how I have ordered the list, they can tell what I am most worried about, and they might even have some advice for me about how I might realign that ordering based on their own concerns.
- I can sign out to my colleagues by running the problem list for each patient, and I know I have covered everything.
- All the diagnosis codes associated with the problems become available (in my EMR) to select in the billing process. And if the patient goes to an outpatient visit, those codes are also available there.
That’s why I love it. It saves time and ensures that nothing gets missed. It helps in communication. It rises above the tangled mass of notes and results and images to give me (and anyone else who cares) a concise picture of what the patient is dealing with, and how we are trying to help.
It’s a bit like the Getting Things Done approach that David Allen and others espouse, which I’ve been trying to master in my non-clinical work for the past decade. The GTD philosophy is that we are most productive when we move all of our “to do” lists and projects out of our minds and into a system so that we can use our brain for what it is good for (focusing on one thing at a time) rather than what it is not very good at (stressfully juggling long lists of things we need to do). It seems like the problem list might serve well as a way to reduce the stress of having to remember all the things we need to do for a patient, and improve our reliability in taking care of all of those things.
The problem list seems so useful when it’s used well.
But that’s the problem: when it’s not used well, it’s a mess.
Or, more specifically: When the responsibility for managing the problem list is not shared by a broad cross-section of people, it’s a mess. When it’s updated only by a couple of problem-list fanatics like me, it’s great… for a while. But then it falls into disrepair and disinformation in the hands of those who disregard its maintenance. “It’s tedious,” my colleagues say when I suggest that maybe we ought to use this part of our EMR for what it was intended. “Can’t take the tedium.” But copying stuff forward day after day is better somehow? What could be more tedious than that?
As an example of a problem list maintenance problem, consider the following. In March of 2014, I admit a patient to the hospital with this on her problem list:
(I sure hope that this patient has not had continual sepsis for over two years!) A quick click makes this acute problem “Resolved,” but then I notice that the patient has had a dozen ambulatory encounters with this “problem” continually listed as active on the chart over the past 27 months. Wow. And to think the patient could have logged in to our patient portal and seen that diagnosis at any time. Wonder if that would cause any patient/parent concern?
That’s an example of why I also hate the problem list.
Neil Mehta and others hit the nail on the head with a recent commentary in the Journal of General Internal Medicine, EHRs in a web 2.0 world: time to embrace a problem-list Wiki. Everybody contributes to the problem list. No one person is saddled with the tedium. Everyone capitalizes on the information—even the patient. The barrier to the use of the problem list, according to these authors, is that we spend all of our energy creating the note that conforms in the best way possible to the E & M coding guidelines (as we understand them). To a lot of folks, this means blowing in every conceivable fact. Result: Unreadable note. No way to grasp what’s going on with the patient.
I do not blame anyone for wanting to get paid, which in medicine today means creating an E & M-complaint “receipt” for care. But the problem list can be harnessed to help you get paid (by clarifying a rich medical decision-making process), and do so a lot more efficiently, while it also makes our care provision more accurate.
We have to look to –and use — EMR software for the real purposes for which it was intended: a more organized approach to good medical care and medical records. But that’s a harder cultural shift than Larry Weed predicted.
Andy Spooner, MD, MS, FAAP is CMIO at Cincinnati Children’s Hospital Medical Center. A general pediatrician, he practices hospital medicine when he’s not enjoying the work involved in keeping the integrated electronic health record system useful for the pediatric specialists, primary care providers, and other child health professionals in Cincy.

I agree…this is a great article…I also think we would all benefit from everyone attaching meds to problems…another thing that would improve the record but definitely require everyone playing nicely! Thanks for the tip on Balsamiq Mockups!
Thanks, Andy, for hitting all the right points — as usual.
When doctors ask me who is responsible for maintaining the problem list, I always answer the same way: “Yes!” When they ask me what I mean by “Yes!” I tell them that it’s the responsibility of every clinician who sees the patient to keep the problem list as up-to-date as possible. Do I expect a cardiologist to add migraine to the problem list? Probably not (but it would be nice!) I do expect the cardiologist to ensure that all of the problems that she is overseeing are appropriately documented in the problem list. Primary care docs never get any passes, unfortunately.
Andy, thanks for channeling one of my favorite rants!
Fascinating that the first two comments to it are both by friends of mine!
I would like to add to the rant. Why can’t the problem list attribute cause and effect? Why can’t I collapse the PL to core issues for focus as well as explode it like MESH terms to get to the granular level. Right now some EHRs can organize the important content by problem including the Assessments and Plans over time which enables problem oriented review of past visits. And while I’m at it, why can’t we attribute things like medications to more than one problem proportionally? Similarly, the subjective and objective portions of the exam should be attributable to more than one problem and for ease of reading should be able to collapse into a flowing narrative of all subjective comments, followed by all objective findings and a list of problems with assessments and plans. Problem oriented charting should export billable notes as a side line to the main purpose of communicating to the care team and patient/family what was going on with the patient and why. In other words the ideal problem list would be modular and able to self-assemble into a billing form, a narrative form for clinicians and a separate one for patients, as well as able to explode to simple concepts for research.
The Problem Child