News 3/20/14
Saint Peter’s Healthcare System (NJ) selects athenahealth’s athenaOne EHR, PM, and communication system for its 176 hospital- and clinic-based physicians.
American Family Care, which operates 160 urgent care facilities across 26 states, agrees to pay the federal government $1.2 million to resolve allegations that it knowingly submitted claims using billing codes higher than appropriate for the actual service rendered. The case stems from a whistleblower lawsuit filed by one of the organization’s former claims processing directors.
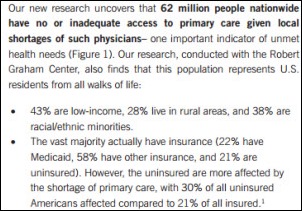
Nationwide 62 million people have no or inadequate access to primary care given local shortages of physicians, according to a report by the National Association of Community Health Centers. Not surprisingly the Association recommends the government provide community health centers with plenty of funding to help address access challenges, but I think the fix requires more than just more money. I’m reminded of a session during HIMSS featuring occasional HIStalk contributor Lyle Berkowitz, MD, who correctly stresses the need for innovation and technology in healthcare to improve access:
If we don’t adopt new technology and change the way we deliver care, it will be harder and harder to get to see a doctor, it will cost more, the rich will cope, the poor will suffer. Many will die earlier than they would have if cost effective treatments were available. We have to act now before the healthcare system goes into meltdown.”
The Drummond Group certifies Kareo EHR for MU 2014 Stage 2.
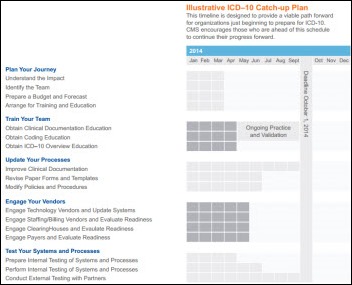
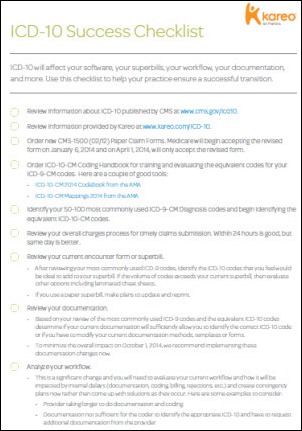
CMS releases Road to 10, a free online resource to help physicians in small practices in their transition to ICD-10. The tool to build an action plan (actually a “catch-up plan”) looks pretty handy and allows providers to customize their roadmap based on practice size, specialty, and the type of technology used in the practice.
Not so surprising findings from a RWJF-funded study: physician practices participating in ACOs tend to be relatively large, members of an IPA or PHO, less likely to be hospital-owned, and more likely to use care management processes and EHRs as compared to practices not participating in ACOs. Researchers found that 61 percent of practices have no plans to participate in ACO, which raises the question of how to get the balance of practices on board with ACOs, if in fact the ACO model proves to provide better and more cost-effective care.
Welcome to new HIStalk Practice Platinum Sponsor Arcadia Healthcare Solutions, which is headquartered just outside of Boston and has additional offices in New York, Seattle, and Nashville. Arcadia provides services and technology for EHR outsourcing; data integration and population analytics; and care delivery transformation and coaching. Clients of the 12-year-old company include five Pioneer ACOs, leading academic medical centers, national health systems, managed care organizations, and several Blues. Arcadia’s advisors can help practices improve key ambulatory network measures 15 to 30 percent in six months by bringing together EHR and claims data and helping providers use it. Some of its EHR optimization accomplishments include reducing log-in time by 50 percent, improving system performance by 27 percent, and increasing physician satisfaction by 20 percent. Arcadia provides expert advisors rather than, as it says, “high-priced management consultants who leave nothing behind but PowerPoint.” Thanks to Arcadia Healthcare Solutions for supporting both HIStalk and HIStalk Practice.
InstaMed launches InstaMed Go, which allows providers to collect patient payments via smartphones from any location with the payments posted automatically to their practice management systems and receipts emailed to patients.
Email Inga.














Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…