From the Consultant’s Corner 9/11/19
Patient Access: Partnering with Clinicians is Essential for Success
By Nancy Gagliano, MD

Nancy Gagliano, MD is CMO at Culbert Healthcare Solutions in Woburn, MA.
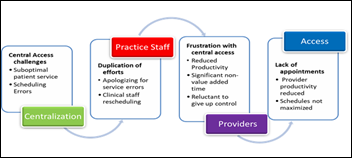
Providers and clinical practices are being persuaded to transition patient access responsibilities to a central patient access center. This comes with the promise of removing administrative burdens for patient scheduling, registration, and more; thus, the practice can focus solely on delivery of care. Patient access center set-up typically transfers existing patient service representatives to a centralized unit, which is organized around pods of specialty expertise. This strategy provides for knowledge transfer to the central unit and a personal link back to the practice. However, in a blink, providers express frustration with scheduling errors and patient complaints. To compound the problem, central staff turnover of around 30% leads to the loss of personal linkages and knowledge transfer.
There are many factors that contribute to an underperforming central access approach, such as inadequate technology and its set up, insufficient and undertrained staff, as well as ineffective management structure. However, complexity of provider scheduling is often an underlying factor severely limiting the potential for success. Organizations often lack standards for provider schedules, visit time, visit types, and protocols. This article provides guidance for an organizational approach to provider scheduling and a partnership between practices and centralized access centers.
We’ve all heard the reasons for complex schedules:
- I need seven minutes for a visit.
- I need 15 minutes for a visit.
- My patients are sicker.
- I shouldn’t waste my valuable expertise outside of my sub-specialty.
- I can only see two – “wellness, consults, annuals, new” in a session.
- My sessions should be three hours.
- My session should be five hours with only 1 new patient.
On top of the scheduling complexity is the “provider bump.” Somehow, conferences, vacations, and car registrations happen at the last minute and patients need to be rescheduled. Altogether, these factors result in gaps in schedules, wrong patients in slots, frequent rescheduling, and unhappy patients and providers.
As a physician, I have frequently seen these challenges, and do not blame the providers. They are trying to bring structure to their chaotic lives in a healthcare world that continues to place more and more burden on them. With long and often unpredictable hours, remembering to submit time-off requests for conferences or to tend to an expired car registration falls to the bottom of their priority lists. Therefore, it is the organization’s responsibility to help provide structure and clear expectations to reduce the chaos.
Time slots
While individual providers have a good sense of how long it typically takes them to see each type of patient, it is extremely challenging for a scheduler to know exactly what type of patient or condition they are scheduling, which often results in placing the patient in the wrong time slot. Additionally, complex schedules will often leave gaps unfilled. If a provider’s schedule has an open 15-minute urgent care slot at 9 am and a 15-minute routine at 11 am, how can a scheduler book a patient requiring a half-hour appointment? When located within an office, a quick chat can provide approval to overbook a timeslot or merge two disparate slots, but a patient access rep often doesn’t have easy access to the practice. Instead of contacting the practice to get authority to adjust a visit type, slots go unfilled. Multiply this by hundreds of providers with their unique scheduling requirements, and it is understandable that scheduling errors occur, and that access is not optimized.
One of the most important endeavors taken by an organization to improve this problem is to establish organization-wide visit-time standards – if not at the organizational level, then at least at each practice level. Our favorite is 20, 40, or 60 minutes per appointment. All patient visit types fit into one of these three-time allotments. The chance of making an error is dramatically reduced, as is the potential for unfilled gaps in the schedule. For providers who see patients faster than this, their schedules can have a few double-booked slots built in, and those providers who take longer have a couple of 20-minute blocks dispersed through their day.
Providers often need some convincing to accept this new template. We advise starting with the total number of patients they currently see during their session and creating the template based on the total volume. Highlight that the patient flow will even out over the day, even if a few patients take longer or shorter than the 20 minutes they were booked for. The result will be far fewer patients booked in incorrect slots and an overall smoother patient flow. As the provider adjusts to the new schedule, blocks or double bookings can be added to further accommodate the provider’s style. To gain provider acceptance, it is important not to initially expect increased provider productivity, but rather reduced scheduling errors and smoother patient flow.
Templates
Scheduling templates are helpful to create a balance of appointment types each day, such as new, annual, follow-up, and urgent. We commonly see two challenges with template approaches. The first is that they are set up with numerous types of appointments, creating rigidity and confusion for the schedulers. Once again this leads to errors. The second is that they are often built on provider choice rather than demand. For example, a provider wants to only see two annual exams daily, but has a panel size requiring four annuals. This results in a cascade of patients put in “wrong” visit types; lack of same day/urgent visits; and frustrated schedulers, providers, and patients.
We recommend an analytic approach to building templates — analyze historic volume, current practice challenges, and build as flexible a template as possible. In addition, while holding slots for certain visit types may be important, such as setting aside new consults, make sure you have a process to unfreeze slots in a suitable time frame for them to be used for other patient needs. For example, many sub-specialists are reluctant to see more general specialty patients, while a health system may have unmet general specialty demand. It may be an appropriate compromise to hold new patient slots for specific disease conditions until three to five days before the date and then open to more general new patients after that.
Protocols
Another common challenge is scheduling protocols that are either too vague or too complex. For example, “back pain” could end up with an orthopedic surgeon, rheumatologist, physical therapist, or primary care provider. The process may not easily facilitate the scheduler matching the patient to the right provider. On the other hand, if the criteria for scheduling is so complex that medical education is needed to decipher it, it may not be appropriate for routine centralized patient access center to schedule. Adding additional clinical staff, or enhanced technology, may be needed for sub-specialty activities. With the right resources to liaison between the practices and central scheduling unit, a middle-ground approach can be devised. It is important to review and develop a formal protocol review process and bring significant variations to the governance body.
Provider Time
Another important component of a successful centralized patient access approach is having provider schedules available for a minimum of six months, and preferably one year out. For this to work, however, call schedules, vacations, and conferences need to be planned and set in advance. A common practice requires providers to submit their time off requests every six to 12 months. With advanced planning, almost all requests can be accommodated. Any additional time-off requests should require practice/department leadership approval. Additionally, finding one’s own coverage and making up the time-off quickly for last minute emergencies should be a standard expectation.
Communication
Whether it’s provider schedules, protocols, or complex patients, there are numerous needs for good communication between the call center and the practices. It is important to have a clear process and expectation for communication. This could be anything from a “back line phone” between the practice and the call center, to a formal liaison relationship. Setting the foundation for a partnership approach requires excellent communication and process to solve problems.
Governance
This all leads to the need for organizational governance. This should include providers, practice management, central access leadership, and IT. Too often, patient access oversight is limited to the operations side of the healthcare system. The clinicians voice their concerns to health system leadership while feeling frustrated and powerless. Health system leadership turns to the central access leaders and demands improvement in accuracy and patient service. All the while, the access center leadership is frustrated by their inability to influence the practices to support their needs. A dyad governance approach is essential for a successful centralized patient access. Both operations and clinical practice representation is essential. It is crucial to develop organizational standards for provider scheduling for everything from visit type, visit length, provider bump rules, to scheduling protocols. In return, the access center should be held accountable for Service Level Agreements, such as abandonment rate, speed to answer, handle time, and accuracy.
In summary, it is unlikely for a centralized patient access approach to be successful without a partnership between centralized patient access and clinical practices. While providers often bristle at standardization, once implemented, providers usually see fewer errors and smoother scheduling. Setting performance expectations of the central access center, as well as implementing scheduling standards, is foundational for a high-performing central access approach. Therefore, creating a dyad governance approach can create both the alignment and the accountability for a successful partnership.
Contacts
More news: HIStalk.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.






Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…