News 5/12/11
RCM provider MDeverywhere acquires Advanced Health Management Services, a provider of practice management and credentialing services. MDeverywhere’s majority shareholder and equity partner Marlin Equity Partners funded the acquisition.
From Black Book Rankings: MED3OOO is named the top-ranked vendor in terms of customer experience and satisfaction among EMR systems for multispecialty clinics. Other top performers include NextGen, Allscripts, Dr. First/Rcopia, Sage, Epic, LSS, and Greenway.
AMGA, whose members include about 300 multi-specialty groups and 67,000 physicians, tells Donald Berwick that 93% of its members would not enroll in an ACO, based on the currently proposed regulatory framework. AMGA President and CEO Don Fisher submitted a letter to Dr. Berwick saying the proposed rule is “overly prescriptive, operationally burdensome, and the incentives are too difficult to achieve to make this voluntary program attractive.” The biggest concerns of members include risk-sharing, static risk adjustment, retrospective attribution, quality measurement, and minimum savings.
Greenway Medical is hosting a free Webinar May 18 entitled The Future of Meaningful Use, EHRs and Accountable Care. It includes an update from Greenway VP Justin Barnes, who is also the former chair of the EHR Association. Greenway also just announced that Childs Medical Clinic (AL) successfully attested its EHR use under Medicare’s Meaningful Use program, the company’s first.
Fredericksburg Nephrology Associates (VA) attests to Meaningful Use using Acumen nEHR version 6.0.
Florida passes a law allowing doctors to be fined $500 if they ask a patient or their parents whether they have a gun in their home. Physicians would also be fined for making a note about gun ownership in a patient’s medical record.
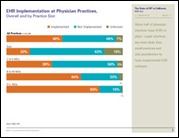
California HealthCare Foundation estimates that 55% of primary care providers in California have implemented electronic medical records. Only 10% of FQHCs claim full EMR implementation, though 47% of community clinics have EMRs. No surprise here: larger practices report higher adoption rates than smaller groups.
CMS is hosting a couple of teleconferences for providers next week, including a May 18 session entitled ICD-10 Conversion Activities. The target audience is medical coders , physician office staff, and health records personnel. On the clinical side, CMS will host a May 19 call on Medicare and Medicaid EHR Incentive Programs: Understanding Meaningful Use.
In case you were wondering, at least 465 ambulatory EHR products have now been ONC-ATCB certified. Good to have options, I suppose.
From 2009 to 2010, the number of healthcare data breaches in healthcare increased from 171 to 761, though the number of documents involved fell from 144 million to 4 million. According to a Verizon Data Breach Investigation report, small- and medium-sized businesses, including physician practices, are considered easy targets for outside hackers because they tend to lack sophisticated technology to protect against attacks.
Aprima reseller Doctors Administrative Solutions (DAS) announces the hiring of 10 employees to accommodate its growth. Over the last six months, DAS has added 22 practices representing about 250 physicians.















Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…